MHF Annual Gathering 2017!
Creating Healing Environments
June 23-25, 2017
Laurelville Mennonite Church Center
Mt. Pleasant, Pennsylvania
Co-hosted with the Mennonite Chaplains Association
Report on Annual Gathering 2017
MHF focuses on Creating Healing Environments at Annual Gathering 2017
Nearly one hundred members of Mennonite Healthcare Fellowship (MHF) gathered at Laurelville Mennonite Church Center over the weekend of June 23-25, 2017 to explore the theme, “Creating Healing Environments.” Severe weather, including torrential downpours and tornado warnings, greeted the attendees at they arrived on Friday, but the weather grew steadily more pleasant as the weekend progressed.
The plenary sessions included meaningful worship experiences, energetic singing, and thought-provoking input by presenters Donna Minter, John Wenger, David Baker, Anthony Brown, and Katerina Friesen. Eight workshops were presented on Saturday afternoon on a variety of topics, with participants able to choose up to four options.
Attendees represented a broad diversity of ages including several families. Twelve children participated in a lively and fun children’s program which met during the adult sessions. A large number of participants were attending their first MHF gathering. Long-time friendships were renewed and new friendships formed over social time, during meals, and between sessions. A highlight of the fellowship was the Saturday evening hymn sing and ice cream social.
For the first time, MHF tried live-streaming the plenary sessions on Facebook. Also created was a short video featuring a number of attendees making brief statements about how they create healing environments in their work. Videos can be viewed on Mennonite Healthcare Fellowship’s Facebook page under the “Videos” tab.
Prior to the Annual Gathering, the MHF Board of Directors met on Thursday evening and Friday morning to consider a number of business items, including discussion about future Annual Gatherings. The consensus of the directors was that an annual meeting is important for maintaining the momentum of the organization, and for providing maximum opportunities for members in various parts of the country to attend. Next year’s Annual Gathering will be June 22-24, 2018, likely in Ohio. The exact location will be shared as soon as a contract with a facility is finalized.
This year’s gathering was co-hosted by the Mennonite Chaplains Association (MCA), of which about a dozen members were present. At their meeting on Friday afternoon, members of MCA voted to disband the organization, citing the difficulty of maintaining a national organization. MCA members are encouraged to become members of MHF, and/or to participate in chaplain cluster meetings sponsored by Mennonite Health Services or denominational chaplain circles. The presence of the chaplains at MHF’s Annual Gathering 2017 enriched the time together. Interim Executive Director Timothy Johnson expressed gratefulness for their attendance. He also expressed special thanks to J. Melvin Janzen, MCA President, for leading a time of centering prayer on Sunday morning before worship.
Annual Gathering 2017 Photo Gallery
Select a picture to start slide show.
Worship and Music Leaders
 Brad Yoder — Music Leader. Pittsburgh-based singer-songwriter Brad Yoder led in music throughout the weekend, and also playing his own songs in a coffeehouse performance Friday night, during the “Snacks & Fellowship” time.
Brad Yoder — Music Leader. Pittsburgh-based singer-songwriter Brad Yoder led in music throughout the weekend, and also playing his own songs in a coffeehouse performance Friday night, during the “Snacks & Fellowship” time.
 Kayla Berkey — Worship Leader, Chair of Worship Commission at Pittsburgh Mennonite Church led the worship time.
Kayla Berkey — Worship Leader, Chair of Worship Commission at Pittsburgh Mennonite Church led the worship time.
Plenary Session Presentations
Friday evening, June 23 – Opening Plenary
 Engaging the Anabaptist Vision: Healing in the Way of Jesus
Engaging the Anabaptist Vision: Healing in the Way of Jesus
Donna Minter
Saturday morning, June 24
 Healing Spaces within 21st Century Healthcare Systems
Healing Spaces within 21st Century Healthcare Systems
John Wenger
Saturday evening, June 24
David Baker
Sunday morning, June 25
 Healing through Sharing Song and Story
Healing through Sharing Song and Story
Tony Brown
 Leaves for the Healing of the Nations: Addressing the Spiritual Roots of the Climate Crisis
Leaves for the Healing of the Nations: Addressing the Spiritual Roots of the Climate Crisis
Katerina Friesen
Workshop Sessions
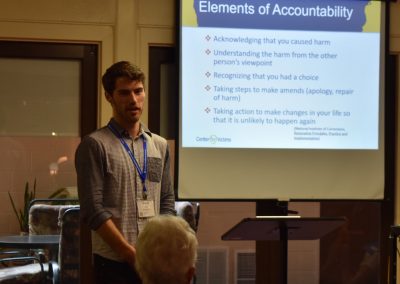
- Introduction to Strategies for Trauma Awareness and Resilience (STAR) – Donna Minter
- Repairing the Breach: Churches as Sites of Environmental Healing and Food System Change – Katerina Friesen
- One Disease: Redox Imbalance as the Root Cause of Chronic Disease – Michael Sherer
- Restoring Trauma-Informed Care: Keeping Ourselves Accountable with Cultural Humility and Social Consciousness – Aaron Erb
- Training in the Healing Professions – Randy Longenecker, Shari Leidig Holland, and panel
- Aging: A time for family conversations—and healing – Marlene and Gerald Kaufman
- Healing Conversations around Contentious Subjects – Kenton Derstine
- Mobilization for Service Reports – Grant Recipients
More information
Essay Scholarship
Students, residents, and other professionals in training were encouraged to submit an essay (under 2,000 words) on the theme “Creating Healing Environments” from their respective perspectives and experiences. Awards and publication were given to the following persons:






















































 Paul D. Leichty, MDiv
Paul D. Leichty, MDiv Kenton T. Derstine
Kenton T. Derstine Indigo Miller, BSN, RN
Indigo Miller, BSN, RN